Introduction
Heel pain, which is also commonly known as Plantar Fasciitis or Plantar Fasciopathy, is an extremely painful and potentially debilitating condition affecting athletic and non-athletic populations.
Characterised by a stabbing pain in the heel which is made worse with weight-bearing, prolonged periods on your feet or increased walking and running with Plantar fasciitis can be extremely difficult to treat.

Thankfully, due to an increased understanding of load modifications, the importance of exercise therapy and highly effective interventions such as Shockwave therapy, heel pain treatment interventions and successful outcomes are on the rise.
What is the Plantar Fascia?
Basic Anatomy
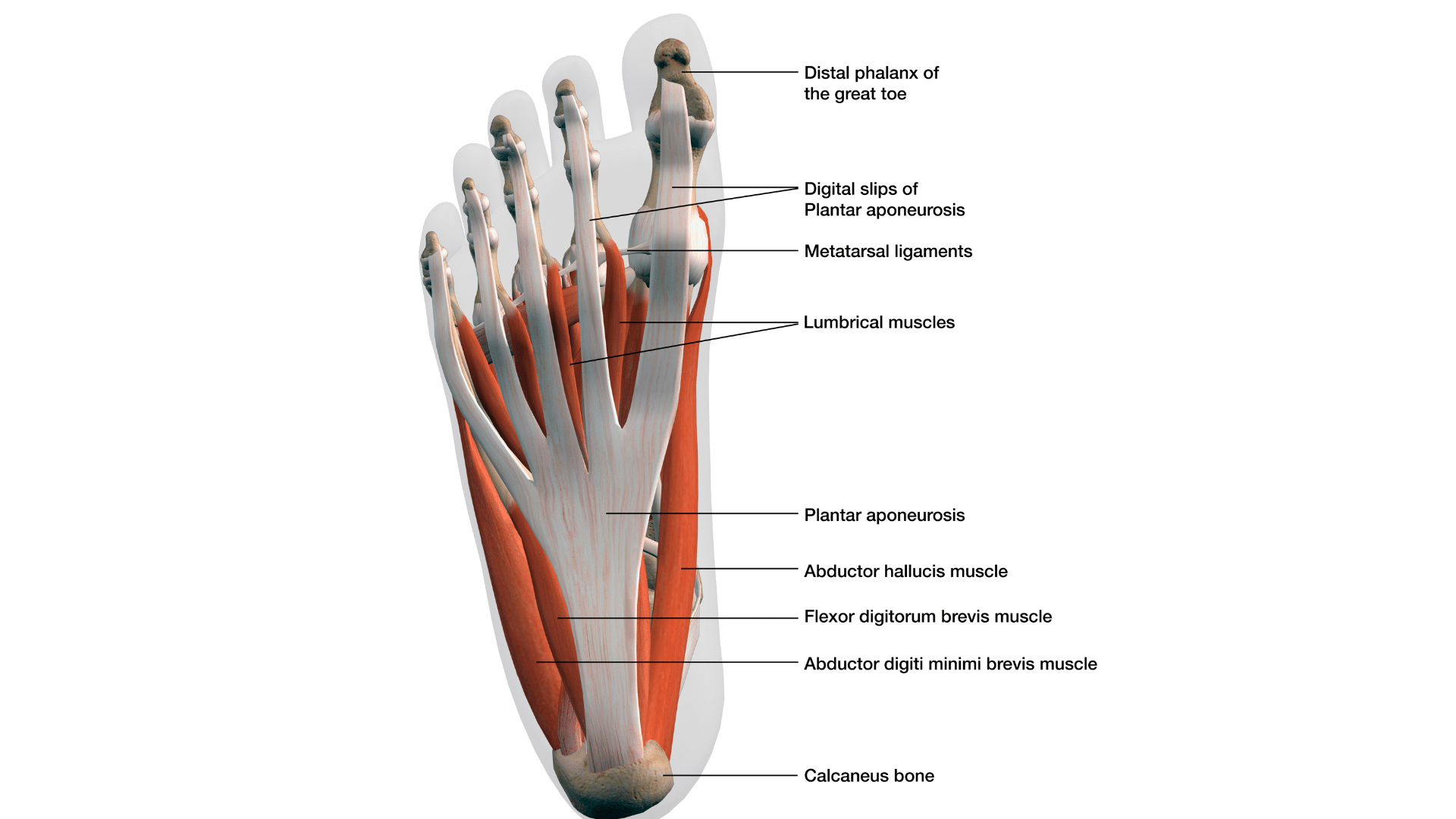
The plantar fascia is a band of tissue (fascia) that connects your heel bone (Calcaneus) to the base of your toes. It supports the arch of the foot and is a shock absorber when walking. This thick spring-like structure is designed to absorb force and return energy to the gait cycle to maximise efficiency when walking and running and reduce pressure.
Sharing fascial attachments with the calf muscles enables this tissue to transmit forces effectively from the musculature at the back of the leg across the sole of the foot. The plantar fascia attaches in two distinct bundles on the medial and lateral aspects of the calcaneus to provide support to the longitudinal arches of the foot.
Despite its name being misleading, the Plantar Fascia is a ligament; ligaments of course connect bone to bone and are designed to provide stability. Considering the complex anatomy of the foot and the huge number of joints and bones which the plantar fascia crosses in the mid and forefoot in particular, it is no surprise that pain and injury to the structure can cause such dysfunction in all aspects of life when Plantar fasciitis is diagnosed.
Complex Anatomy
The central part of the plantar fascia forms the plantar aponeurosis, which starts proximally at the calcaneus and extends distally into five separate bands that become the digital sheaths. It is supported inferiorly by the superficial transverse metatarsal ligament.
The fascia acts as a border for the five anatomic compartments of the foot, which include the medial compartment, the central compartment, the lateral compartment, the dorsal compartment, and the interosseous compartment.
The fascia plays a crucial role in dividing and attaching muscles in the foot. The relationship of the fascia with the muscles can be further described by the compartment they are in.
Medial compartment: The medial plantar fascia overlies the abductor hallucis, flexor hallucis brevis, and the flexor hallucis longus tendon.
Central compartment: The central plantar fascia overlies the flexor digitorum brevis, the tendon of the flexor hallucis longus, the tendons and musculature of the flexor digitorum longus, the quadratus plantae, the lumbricals, and the adductor hallucis.
Lateral compartment: The lateral plantar fascia overlies the abductor and flexor digiti minimi brevis.
Interosseous compartment: The plantar and dorsal interosseous fascias border the interosseous muscles.
Dorsal compartment: The dorsal fascia overlies the extensors hallucis brevis and extensor digitorum brevis.
It is clear that the complex inter-relationship of so many anatomical structures is unlikely to be solved by simple interventions alone. This is why the management of Plantar fasciitis is multi-faceted with an appreciation of biomechanics considered vital for successful outcomes. Whilst interventional techniques can achieve short-term relief, long-term improvements can only be maintained through a thorough treatment package underpinned by foot and ankle strength.

What is the main cause of plantar fasciitis (aka What is the main causes of heel pain)?
Heel pain as a collective can be due to a number of factors such as bone spurs, heel spurs or bursitis but there is no doubt that the most common cause is plantar fasciitis. “Itis” refers to inflammation and therefore in simple terms heel pain is caused by inflammation of the plantar fascia.
In recent years, research has suggested that not all Plantar fasciitis has an active inflammatory component and as such the term Plantar Fasciopathy was used interchangeably. This terminology was felt to be more reflective of the continuum of fascia dysfunction which may include inflammation but may also be due to pathological changes within the structure itself leading to micro-tearing and fibre dysfunction.
Plantar fasciitis pain is caused by an overloading of the fascia at the insertion onto the heel bone. Particularly affecting the medial insertion (often the most painful part on palpation) this overload results in local inflammation. This inflammation could occur acutely if an individual was to suddenly increase the load on the fascia and subsequently develop plantar fasciitis.
An increase in load could occur due to an increase in walking distance, running distance, standing, specific gym work involving repeated jumping (eg skipping) or due to a change in a person’s physical attributes such as an increase in weight.
Typically a “sore heel” after an increase in load will settle with rest after just a few days with advice on supportive shoes and avoiding flip flops and high heels (!), however on occasion, chronic pain or plantar fasciitis develops and despite rest, the initial pain doesn’t resolve or becomes easily irritated by any return to load bearing activity. These are the tricky foot problems which need more detailed treatment plans from a physio or physical therapist.
When tissues become dysfunctional, and following the (potentially recurrent) long periods of acute inflammation, they can become ineffective at doing their job. Normally the fibres of the plantar fascia (in keeping with their role as a large spring-like structure) will be aligned in a way to absorb and transmit forces in keeping with their tensile properties.
When pathology (Fasciopathy) develops the fascia becomes thickened and swollen, the fluid within the fascia impacts the load-bearing capabilities of the structure and over time the tensile properties of the fascia are reduced through poor alignment of the fascial fibres.
It is easy to see at this point how we are essentially stuck on a vicious circle of:
Inflammation – Overload – Reduced loading capability of Plantar Fascia – Inflammation.
Treating plantar fasciitis then becomes about breaking that cycle and restoring the physical qualities of the structure whilst allowing adequate time to reduce heel pain and inflammation.
This could be achieved with simple advice such as the appropriate application of an ice pack and medication, footwear changes or advice to lose weight but in reality, is likely to need a little more detail.
Severe heel pain is one of the most difficult conditions to get on top of, its location on the sole of the foot means it is often felt with the very first step of the day when getting out of bed (indeed the level of pain at this moment will usually be recorded as a method of measuring improvement).
We understand that foot pain on waking is a miserable thing to experience and plantar fasciitis pain can in turn become the first thing we think about in the morning; that is why it is important to diagnose plantar fasciitis as soon as possible in order that effective advice and treatment can be commenced as soon as possible.

Diagnose plantar fasciitis
Diagnosis of plantar fasciitis can be made following an in-depth history and subjective assessment with a Physiotherapist or Sports and Exercise Medicine Consultant. The R4P Heel Pain service based in Liverpool was set up to guide you through this often complex condition and can be accessed here. https://rehab4performance.com/services/the-r4p-heel-pain-service/ with a summary of the services offered below.
Management –
1. Accurate diagnosis (including Ultrasound scanning with a Doctor) and prognosis planning
2. Load and activity modification
3. Advice on medication
4. Appropriate therapeutic modalities and treatment interventions
5. Extracorporeal shockwave therapy
6. Footwear/insole modification
7. Bespoke exercise program to stretch and strengthen appropriate tissues to restore the load-bearing capabilities of the foot and ankle complex within a comprehensive lower body conditioning program
8. On occasion, injections or referral to a foot and ankle specialist may be required to progress recovery
9. We will guide you through all the relevant pathways depending on the diagnosis
The complete approach to Heel pain (in detail)
Accurate Diagnosis and Prognosis
Like most issues, the first step (no pun intended) is to get an accurate diagnosis. Whilst most heel pain issues are due to Plantar fasciitis there are occasions when other issues can cause the pain and would require a different approach.
A diagnosis can be reached via in-depth subjective and objective assessment of the painful region and where appropriate Ultrasound imaging can be carried out. Ultrasound allows the Doctor to visualise and measure the plantar fascia which in the case of plantar fasciitis will be thickened and swollen, tiny tears within the fascia can also be identified.
Load and Activity Modification
We understand that people want to keep doing what they enjoy most. We recognise the impact of exercise on mental health and well-being. As such we will do everything to keep our patients as active as possible during the rehabilitation program, On occasion however, it may be necessary to modify loading (such as distance walked or run) in order to get on top of any acute flare-ups in symptoms of plantar fasciitis.

On other occasions, we will also guide your return to increasing mileage in a graded and sustained way to gradually expose the recovering tissue to loading and keep you back doing what you enjoy doing. This would all be part of our comprehensive approach to heel pain management, once it’s gone we want to do everything possible to prevent plantar fasciitis and the key lies in load management alongside strength and power improvement.
Advice on medication
Where appropriate we can advise on pain relief and the use of NSAIDs (non-steroidal anti-inflammatories) to help with symptoms, reduce swelling and provide us with a therapeutic window for effective exercise intervention.
Appropriate therapeutic modalities and treatment interventions
There are many treatment interventions which have been shown to be effective in the treatment of heel pain and plantar fasciitis. Whilst there aren’t many quick fixes it is true that targeted stretching exercises, mobilising exercises, joint mobility work and soft tissue release for the foot and calf muscles can have therapeutic benefits to relieve pain. Where these are appropriate we will target the source of pain and advise you of the exercises you need to be doing on a daily basis.
Extracorporeal Shockwave Therapy (Shockwave).
In recent years a huge body of evidence has shown that Shockwave is one of the most effective treatments for heel pain and plantar fasciitis. Whilst it isn’t clear why it has been so effective we can make a few assumptions based on what we know about the pathology.
Shockwave (as the name suggests) delivers targeted pulses of force to injured and painful tissues. The plantar fascia at its point of attachment onto the heel is likely to adapt to this force by developing more tensile strength to cope.
The Shockwave treatment is typically delivered one week apart with gradually increasing forces and over time this is associated with a gradual reduction in pain. Three shockwave treatments are usually carried out as part of a longer-term rehabilitation program.
Chronic heel pain and plantar fasciitis commonly are slow to resolve and it’s important that any practitioner you deal with is honest about the likely timescales. Quick fixes are likely to be short-lived with long-term improvements needing a more consistent and sustained approach.
Footwear and Insoles
Our feet weren’t designed to wear shoes and be stuffed inside the shoes and boots of the modern day, at some point in human evolution we were happily wandering around in bare feet. Barefoot walking, running and training have gained some interest and momentum in recent years with a recognition that a foot outside of the constraints of footwear will become stronger over time and more connected to the rest of the body (in particular the lower limb).
A sudden change to barefoot activity is likely to lead to problems if not carefully introduced however an introduction to barefoot activity will be an important part of any exercises designed to load the bottom of your foot. Quite simply a well-cushioned trainer gives the arch of your foot the maximum excuse to do very little and be really quite lazy!
Feet come in all shapes and sizes and where appropriate advice on footwear and insoles can make a huge difference in terms of pain relief and long-term improvement. When required, we will refer to Podiatry for further assessment and bespoke insole (shoe inserts) provision to help with arch support, offload of painful structures and biomechanical enhancement.
Bespoke Exercise Program
The aim of the bespoke exercise program in the treatment of heel pain and plantar fasciitis is to rebuild the physical qualities of the plantar fascia, foot and lower limb, in general, to cope with the demands of the individual whilst trying to decrease inflammation and maximise performance.
This program will be a combination of targeted stretching, strengthening exercises and increasingly complex movement tasks to enable the foot to cope under various positions of strain.
Depending on what the individual is working back to, be it wanting to walk the dog for a few miles each day, training for a marathon or returning to top-level football, rugby or dancing will determine what the end-stage exercise program looks like.
The program will be built for you.

Injections for plantar fasciitis and Injections for heel pain
On occasion and depending on the presenting pathology identified on imaging it may be appropriate for an injection to be used to treat the plantar fasciitis. In the past, steroid injections were used to treat plantar fasciitis and were hugely effective in reducing pain, however, they were often short-lived in terms of effectiveness and in active individuals in particular led to soft tissue breakdown and potential rupture of the plantar fascia.
The risks associated with an injection would always be considered in relation to the individual’s case.
Referral to a Foot and Ankle Surgeon or Specialist
On occasion, we refer to a foot and ankle surgeon for a second opinion or specialist review. We have close contacts with surgeons all over the country and in Liverpool, we are proud to partner with https://www.liverpoolfootandankle.com/prof-lyndon-mason for rapid access to his expertise.
Expert guidance
We recognise that heel pain is a debilitating condition and the complex nature of the symptoms is only matched by the seemingly endless list of possible solutions. Our job is to guide you through the options and walk the journey with you.
Where a quick solution is required we will discuss the risks and benefits and when a long-term solution is required we will advise accordingly where we can help and where further specialist opinion is required.
We have access to unique equipment such as our Alter-G for gradual loading of injured tissue, this enables those with heel pain to experience pain-free walking and running via a reduction of body weight on this unique piece of equipment and a gradual introduction of weight over time – a priceless piece of kit.
Beyond this our Strength and Power assessments using Isokinetic Dynamometry and Force Plates enable us to target exactly the physical components required to turn the condition around, maybe the individual is strong but lacks the reactive strength required to transmit that strength up the kinetic chain.
We can identify and target accordingly.
To sum up…
If you are suffering from heel pain we hope this blog has given you hope that all isn’t lost and solutions do exist with perseverance and honesty about what each can achieve!
Hopefully, you know more about what causes plantar fasciitis to flare up, plantar fasciitis treatment, plantar fasciitis relief, plantar fasciitis remedy and fasciitis meaning.
We hope to have informed you about orthotics, plantar fasciitis cause, plantar fasciitis meaning, where is plantar fasciitis pain located and recovery time along with the benefits of a podiatrist, treatments, nonsurgical treatment and calf stretching!
It’s a tricky condition and needs expert help and guidance, contact us here at R4P Liverpool and take the first steps to pain-free steps again.